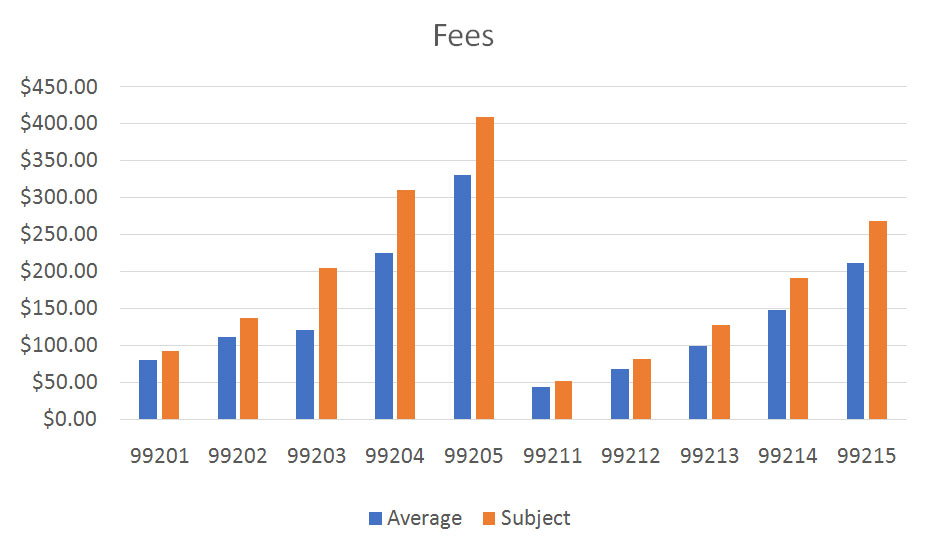
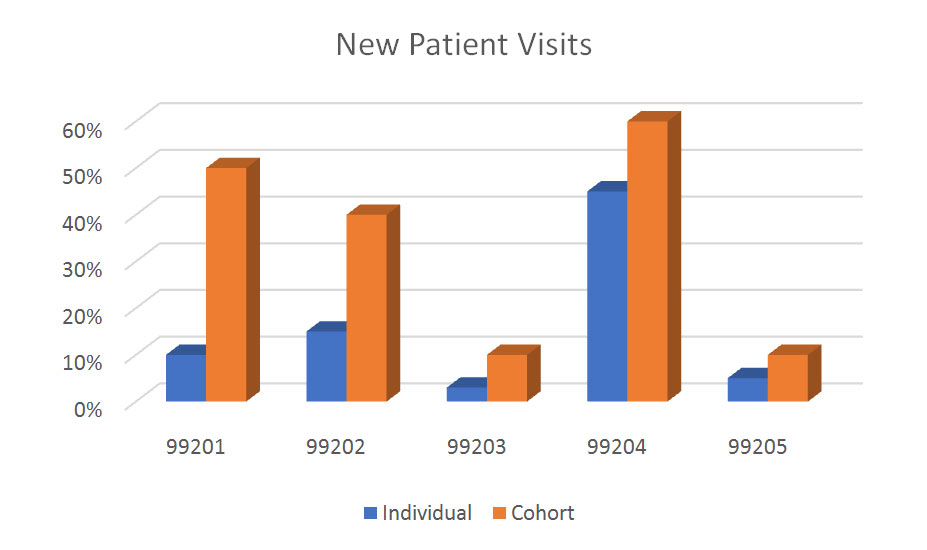
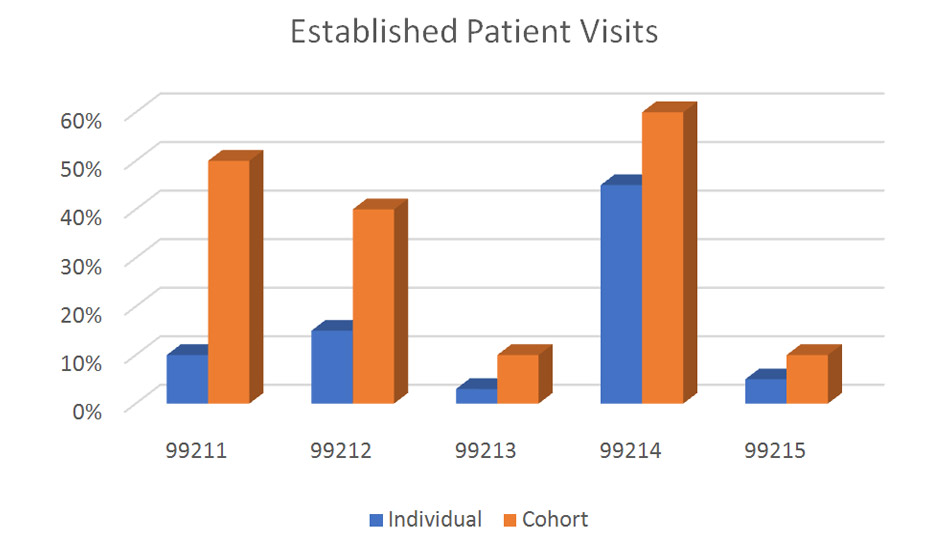
As payers move towards a greater integration of quality and performance data into the payment process, it is increasingly important for providers to know and understand their performance metrics. Quality indicators are frequently submitted alongside of charges, and the CPT codes used to describe services rendered are vitally important. Payers use this data when determining costs associated with episodes of care, and include provider charges and payments alongside the facility charges and payments to arrive at total charges and costs or a given therapeutic or diagnostic intervention.
Every provider should know how their services are characterized when submitter to payers, and how their use of CPT codes compare to other, similar providers. HCS reduces most of this information into easily understood graphics, such as those shown below.
The summary data includes only office visit codes, but many specialties have other frequently-used CPT codes, and there are also included as appropriate. Dermatology, for example, would compare utilization for CPT’s 11100, 11101, 11301, 17000, 12031 and/or other codes as may be indicated.